Automatic Breathing Unit
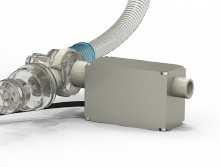
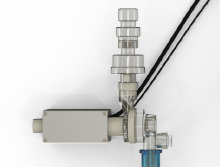
ABU is a CE-marked medical device that transforms the traditional AMBU device into a real mechanical ventilator, for ICU, through the implementation of advanced flux and pressure sensors and a high-precision feedback system. ABU can be used for both invasive and non-invasive ventilation.
Covid-19
emergency
ABU functions as a
highly flexible tool for the
management of patients
in different phases of
treatment.
Entering
ICU
Facilitates the critical
first phase of ventilation
to intubated patients
waiting for a standard
ventilator.
Discharge
from ICU
Provides extubated
patients with assisted
breathing while they
resume normal breathing
(weaning post-ARDS).
ABU IS IDEAL FOR EMERGENCY SCENARIOS WHERE THE SET UP OF MECHANICAL VENTILATION IS COMPLEX.

The Advantages
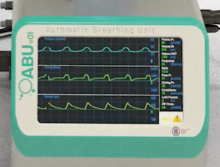
ABU allows users to electronically monitor and control the following functions
• PEEP
• Peak Inspiratory Pressure
• Airflow
• Breathing frequency
• I:E ratio
• Tidal volume
• Plateau Pressure
• Support Pressure
• FiO2 (21%, 45%, 99%).
• Assisted ventilation
• Connection to centralized alarm system
• Data transfer
• Battery autonomy: 1,30 h.
• Touch screen 7” interface
It is possible to use the device in trigger mode for weaning the patient during recovery until
normal breathing is achieved.
| Configurable Parameters | Min Value | Max Value |
|---|---|---|
| BREATH FREQUENCY | 8 resp. acts/min | 35 resp. acts/min |
| TIDAL VOLUME | 50 ml | 1.500 ml |
| I:E Ratio | 1 : 1 | 1 : 4 |
| MAX CONTROLLABLE PRESSURE | 0 cm H2O | 60 cm H2O |
| PEEP PRESSURE | 0 cm H2O | 20 cm H2O |
Monitored parameters
PEEP pressure
The term PEEP refers to the end-expiratory pressure that is applied to the patient when ventilated with invasive or non-invasive mechanical support. Generally the end exhalation pressure in a healthy lung is 0 cm H2O, but when PEEP is applied, this pressure is increased; PEEP is generally used when there are some specific lung problems, which lead to collapse of the alveoli and peripheral airways.
Peak pressure
Maximum airway pressure reached during insufflation.
Air flow
Volume of air passing through a duct in the time unit. It is generally measured in L/min o L/sec.
Tidal Volume
Volume of air entering or leaving the respiratory system during each normal respiratory cycle
Respiratory frequency
Number of respiratory acts per minute
Inhalation/expiration ratio (I:E)
This report expresses how the respiratory period is divided into its two components: inspiratory time and expiratory time. In spontaneous breathing in healthy patients, inspiratory and expiratory time are roughly equivalent: I:E=1:1. In mechanical ventilation the inspiratory phase is usually kept shorter than the expiratory phase to allow the entire current volume to escape from the lungs (I:E=1:2). When there are serious oxygenation problems, an inverted I:E ratio (I:E=2:1) may help to improve oxygenation
Pressure Trigger
The trigger is defined inspiratory when it starts the inspiratory and expiratory phase when it activates the “cycling” of the machine at exhalation. In assisted or spontaneous ventilation the inspiratory trigger can be pressure or flow. The pressure trigger compares, instant by instant, the pressure detected with the threshold set by the operator and when the two values coincide the machine will pressurize the airways giving rise to the inspiration.
Flow Trigger
The trigger is defined inspiratory when it starts the inspiratory and expiratory phase when it activates the “cycling” of the machine at exhalation. In assisted or spontaneous ventilation the inspiratory trigger can be pressure or flow. The flow trigger is based on the principle of a continuous flow in the circuit that is constantly read by flow sensors present in the inspiratory and expiratory pathway and compared with the threshold value set by the health care workers.
Backup ventilation
Forced ventilation that the system performs in case it does not detect a spontaneous respiratory act of the patient.
Configurable parameters
From a minimum of 8 to a maximum of 30 acts/minute
From a minimum of 200 ml to a maximum of 1.500 ml
From a minimum ratio 1:1 to a maximum ratio 1:4











